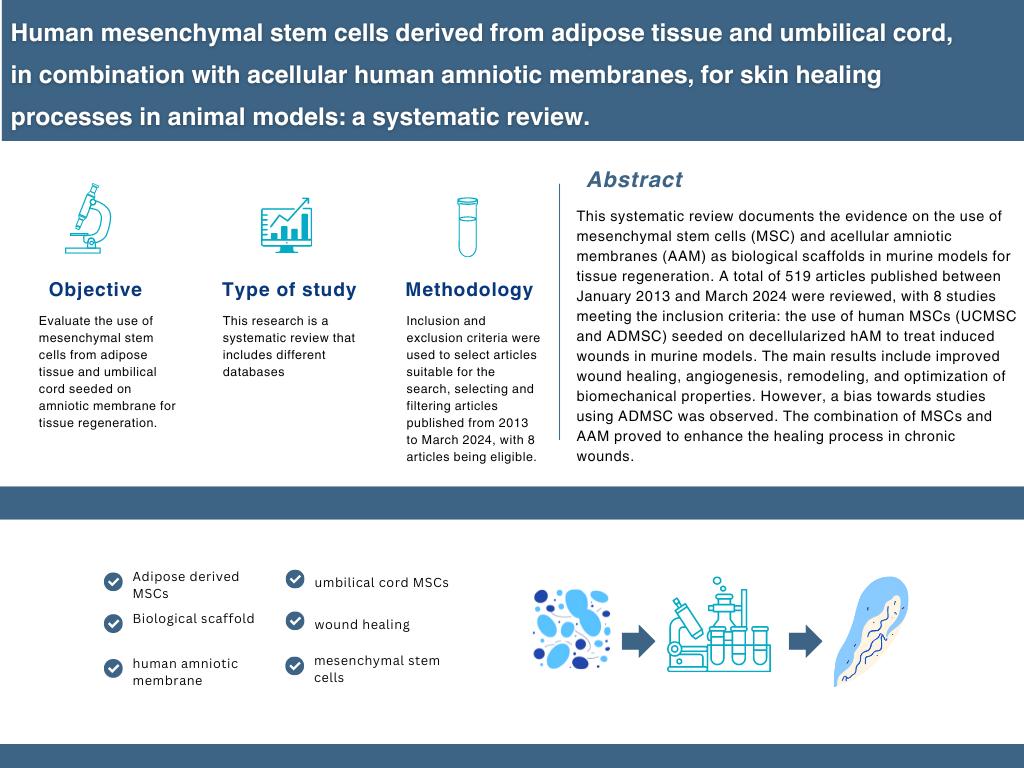
Human Mesenchymal Stem Cells Derived from Adipose Tissue and Umbilical Cord, in Combination with Acellular Human Amniotic Membranes, for Skin Healing Processes in Animal Models: a Systematic Review
DOI:
https://doi.org/10.17488/RMIB.45.3.3Keywords:
adipose-derived MSCs, biological scaffold, human amniotic membrane, mesenchymal stem cells, umbilical cord MSCs, wound healingAbstract
This systematic review aims to document the available research evidence regarding using mesenchymal stem cells (MSCs) and acellular amniotic membranes (AAM) as scaffolds in the murine model for tissue regeneration. This research was developed by analyzing available information on databases like Google Scholar, Pubmed, Scopus, and Web of Science, using the following key terms ''Human Stem Cells'', ''Amniotic membrane'', ''Wound healing' ' and ''Animal model''. A total of 519 articles published from January 2013 to March 2024 were found, but only 8 studies were included in this review, the inclusion criteria were as follows the use of human-derived stem cells (UCMSCs and ADMSCs) seeded in decellularized hAM, in murine models with induced wounds (incisions or burns); exclusion criteria: stem cells obtained from non-human origin, combination of human stem cells from different tissues, use of a different biological scaffold, and studies that not assess efficacy in skin regeneration. The main outcomes were decreased wound closure time, increased angiogenesis, remodeling and increase in extracellular matrix deposition, increased synthesis of growth factors and anti-inflammatory cytokines, and optimization of biomechanical properties. Moreover, one of the main findings was that combining these methods can improve the healing process in chronic wounds. The main bias was related to the inclusion of more studies that used ADMSC (5 of 8); additionally, there were differences in the animal model used, the induced wound, and the comparison of different variables between the studies. In conclusion, we found that the combination of MSCs and AAM as a bio-scaffold improves general tissue healing and regeneration.
Downloads
References
] D. Queen and K. Harding, “What’s the true costs of wounds faced by different healthcare systems around the world?,” Int. Wound J., vol. 20, no. 10, pp. 3935–3938, 2023, doi: https://doi.org/10.1111/iwj.14491
S. Bowers and E. Franco, “Chronic Wounds: Evaluation and Management,” Am. Fam. Physician, vol. 101, no. 3, pp. 159-166, 2020. [Online]. Available: https://www.aafp.org/pubs/afp/issues/2020/0201/p159.html
K. Las Heras, M. Igartua, E. Santos-Vizcaino, and R. M. Hernandez, “Chronic wounds: Current status, available strategies and emerging therapeutic solutions,” J. Control. Release, vol. 328, pp. 532–550, 2020. doi: https://doi.org/10.1016/j.jconrel.2020.09.039
A. M. Jorgensen, M. Varkey, A. Gorkun, C. Clouse, et al., “Bioprinted Skin Recapitulates Normal Collagen Remodeling in Full-Thickness Wounds,” Tissue Eng. Part A, vol. 26, no. 9–10, pp. 512–526, 2020, doi: https://doi.org/10.1089/ten.tea.2019.0319
R. D. Galiano, O. M. Tepper, C. R. Pelo, K. A. Bhatt, et al., “Topical vascular endothelial growth factor accelerates diabetic wound healing through increased angiogenesis and by mobilizing and recruiting bone marrow-derived cells,” Am. J. Pathol., vol. 164, no. 6, pp. 1935–1947, 2004, doi: https://doi.org/10.1016/s0002-9440(10)63754-6
C. K. Sen, “Human Wound and Its Burden: Updated 2020 Compendium of Estimates,” Adv. Wound Care, vol. 10, no. 5., pp. 281–292, 2021. doi: https://doi.org/10.1089/wound.2021.0026
V. Sabapathy, B. Sundaram, S. V. M., P. Mankuzhy, and S. Kumar, “Human wharton’s jelly mesenchymal stem cells plasticity augments scar-free skin wound healing with hair growth,” PLoS One, vol. 9, no. 4, 2014, art. no. e93726, doi: https://doi.org/10.1371/journal.pone.0093726
A. Hassanshahi, M. Hassanshahi, S. Khabbazi, Z. Hosseini-Khah, et al., “Adipose-derived stem cells for wound healing,” J. Cell. Physiol., vol. 234, no. 6, pp. 7903–7914, 2019, doi: https://doi.org/10.1002/jcp.27922
L. Mazini, L. Rochette, B. Admou, S. Amal, and G. Malka, “Hopes and limits of adipose-derived stem cells (ADSCs) and mesenchymal stem cells (MSCs) in wound healing,” Int. J. Mol. Sci., vol. 21, no. 4, 2020, art. no. 1306, doi: https://doi.org/10.3390/ijms21041306
A. R. Khalatbary, M. Omraninava, D. Nasiry, M. Akbari, et al., “Exosomes derived from human adipose mesenchymal stem cells loaded bioengineered three-dimensional amniotic membrane-scaffold-accelerated diabetic wound healing,” Arch. Dermatol. Res., vol. 315, no. 10, pp. 2853–2870, 2023, doi: https://doi.org/10.1007/s00403-023-02709-z
B. A. Aguado, W. Mulyasasmita, J. Su, K. J. Lampe, and S. C. Heilshorn, “Improving viability of stem cells during syringe needle flow through the design of hydrogel cell carriers,” Tissue Eng. Part A, vol. 18, no. 7–8, pp. 806–815, 2012, doi: https://doi.org/10.1089/ten.tea.2011.0391
J. Elango, C. Zamora-Ledezma, and J. E. Maté-Sánchez de Val, “Natural vs Synthetic Polymers:
How Do They Communicate with Cells for Skin Regeneration—A Review,” J. Compos. Sci., vol. 7, no. 9, 2023, art. no. 385, doi: https://doi.org/10.3390/jcs7090385
G. Satchanska, S. Davidova, and P. D. Petrov, “Natural and Synthetic Polymers for Biomedical
and Environmental Applications,” Polymers, vol. 16, no. 8, 2024, art. no. 1159, doi: https://doi.org/10.3390/polym16081159
] A. L. Ingraldi, R. G. Audet, and A. J. Tabor, “The Preparation and Clinical Efficacy of Amnion-Derived Membranes: A Review,” J. Funct. Biomateri., vol. 14, no. 10, 2023, art. no. 531, doi: https://doi.org/10.3390/jfb14100531
Z. Zhou, J. Xun, C. Wu, C. Ji, et al., “Acceleration of burn wound healing by micronized amniotic membrane seeded with umbilical cord-derived mesenchymal stem cells,” Mater. Today Bio., vol. 20, 2023, art. no. 100686, doi: https://doi.org/10.1016/j.mtbio.2023.100686
S. Doudi, M. Barzegar, E. A. Taghavi, A. Ehterami, et al., “Applications of acellular human amniotic membrane in regenerative medicine,” Life Sci., vol. 310, 2022, art. no. 121032, doi: https://doi.org/10.1016/j.lfs.2022.121032
V. Moghimi, J. Rahvarian, Z. Esmaeilzadeh, N. Mohammad-Pour, et al., “Adipose-derived human mesenchymal stem cells seeded on denuded or stromal sides of the amniotic membrane improve angiogenesis and collagen remodeling and accelerate healing of the full-thickness wound,” Acta Histochem., vol. 125, no. 3, 2023, art. no. 152027, doi: https://doi.org/10.1016/j.acthis.2023.152027
H. R. Aghayan, M. S. Hosseini, M. Gholami, F. Mohamadi-Jahani, et al., “Mesenchymal stem cells’ seeded amniotic membrane as a tissue- engineered dressing for wound healing,” Drug Deliv. Transl. Res., vol. 12, no. 3, pp. 538–549, 2022, doi: https://doi.org/10.1007/s13346-021-00952-3
S. Xiao, C. Xiao, Y. Miao, J. Wang, R. Chen, Z. Fan, Z. Hu, “Human acellular amniotic membrane incorporating exosomes from adipose-derived mesenchymal stem cells promotes diabetic wound healing,” Stem Cell Res. Ther., vol. 12, no. 1, 2021, art. no. 255, doi: https://doi.org/10.1186/s13287-021-02333-6
S. S. Hashemi, M. R. Pourfath, A. Derakhshanfar, A. Behzad-Behbahani, and J. Moayedi, “The role of labeled cell therapy with and without scaffold in early excision burn wounds in a rat animal model,” Iran J. Basic Med. Sci., vol. 23, no. 5, pp. 673–679, 2020, doi: https://doi.org/10.22038/ijbms.2020.34324.8156
W. Minjuan, X. Jun, S. Shiyun, N. Haitao, et al., “Hair Follicle Morphogenesis in the Treatment of Mouse Full- Thickness Skin Defects Using Composite Human Acellular Amniotic Membrane and Adipose Derived Mesenchymal Stem Cells,” Stem Cells Int., vol. 2016, 2016, art. no. 8281235, doi: https://doi.org/10.1155/2016/8281235
P. Chen, M. Lu, T. Wang, D. Dian, Y. Zhong, and M. Aleahmad, “Human amniotic membrane as a delivery vehicle for stem cell-based therapies,” vol. 272, 2021, art. no. 119157, doi: https://doi.org/10.1016/j.lfs.2021.119157
M. Fénelon, S. Catros, C. Meyer, J.-C. Fricain, et al., “Applications of human amniotic membrane for tissue engineering,” Membranes, vol. 11, no. 6, 2021, art. no. 387, doi: https://doi.org/10.3390/membranes11060387
A. Trounson and C. McDonald, “Stem Cell Therapies in Clinical Trials: Progress and Challenges,” Cell Stem Cell., vol. 17, no. 1. pp. 11–22, 2015, doi: https://doi.org/10.1016/j.stem.2015.06.007
E. Mirzadegan, H. Golshahi, and S. Kazemnejad, “Current evidence on immunological and regenerative effects of menstrual blood stem cells seeded on scaffold consisting of amniotic membrane and silk fibroin in chronic wound,” Int. Immunopharmacol., vol. 85, 2020, art. no. 106595, doi: https://doi.org/10.1016/j.intimp.2020.106595
A. M. Murthi and M. Lankachandra, “Technologies to Augment Rotator Cuff Repair,” Orthop. Clin. North Am., vol. 50, no. 1, pp. 103–108, 2019, doi: https://doi.org/10.1016/j.ocl.2018.08.005
A. L. Takejima, J. C. Francisco, R. B. Simeoni, L. Noronha, et al., “Role of mononuclear stem cells and decellularized amniotic membrane in the treatment of skin wounds in rats,” Tissue Barriers, vol. 10, no. 2, 2022, art. no. 1982364, doi: https://doi.org/10.1080/21688370.2021.1982364
S. Iranpour, N. Mahdavi-Shahri, R. Miri, H. Hasanzadeh, et al., “Supportive properties of basement membrane layer of human amniotic membrane enable development of tissue engineering applications,” Cell Tissue Bank, vol. 19, no. 3, pp. 357–371, 2018, doi: https://doi.org/10.1007/s10561-017-9680-z
M. Salazar Dobrosky, “Utilización de membrana amniótica como apósito biológico en quemaduras y heridas cutáneas,” Rev. Med. Sinerg., vol. 7, no. 11, 2022, art. no. e912, doi: https://doi.org/10.31434/rms.v7i11.912
C. L. Insausti, M. Rodríguez, G. Castellanos, and J. M. Moraleda, “Amniotic membrane-derived stem cells: immunomodulatory properties and potential clinical application,” Rev. Hematol. Mex., vol. 15, no. 1, pp. 11–20, 2014. [Online]. Available: https://revistadehematologia.org.mx/article/propiedades-inmunomoduladoras-de-las-celulas-madre-de-la-membrana-amniotica-nuevas-perspectivas/
R. Saleh and H. M. Reza, “Short review on human umbilical cord lining epithelial cells and their potential clinical applications,” Stem Cell Res. Ther., vol. 8, no. 1, 2017, art. no. 222 doi: https://doi.org/10.1186/s13287-017-0679-y
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista Mexicana de Ingenieria Biomedica

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Upon acceptance of an article in the RMIB, corresponding authors will be asked to fulfill and sign the copyright and the journal publishing agreement, which will allow the RMIB authorization to publish this document in any media without limitations and without any cost. Authors may reuse parts of the paper in other documents and reproduce part or all of it for their personal use as long as a bibliographic reference is made to the RMIB. However written permission of the Publisher is required for resale or distribution outside the corresponding author institution and for all other derivative works, including compilations and translations.